
How Long Do Opioids Stay In Your System?
Opioids are a broad classification of drugs that encompasses a wide variety of both licit and illicit substances. There are…

Opioids are a broad classification of drugs that encompasses a wide variety of both licit and illicit substances. There are…
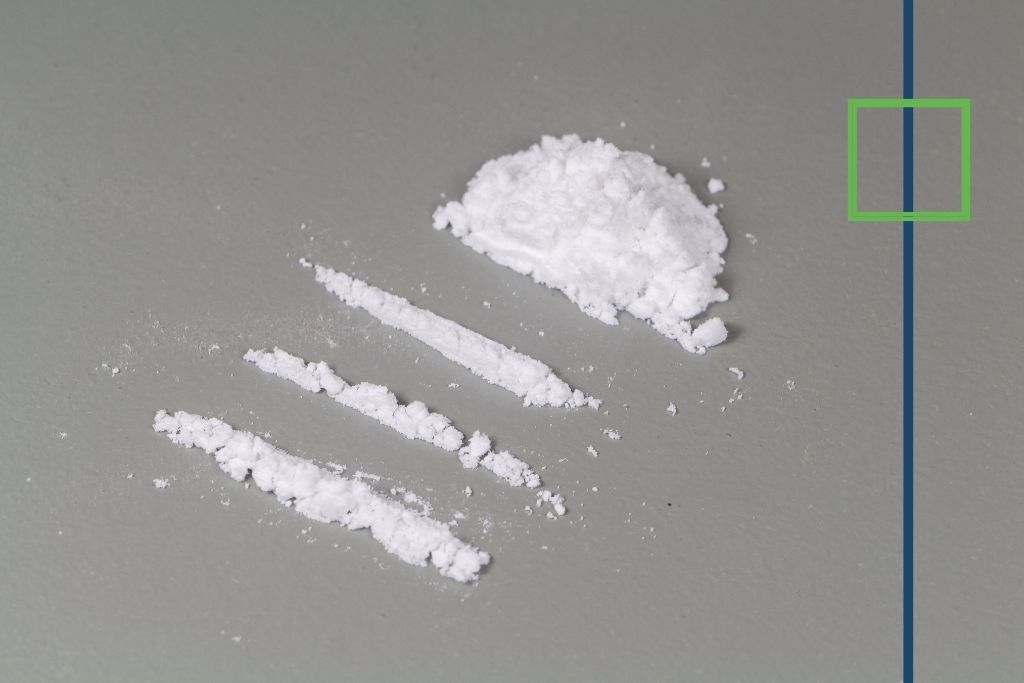
To answer the most pressing question on everyone’s mind: yes, cocaine is very addictive and can lead to addiction even after…

Within a few seconds after taking cocaine, the pupils will enlarge, body temperature will increase as heart rate and blood…
What is Fentanyl and How Is It Used? Fentanyl is a powerful synthetic opioid with a dangerous reputation. It can…

Alcohol withdrawal isn’t pretty; it can trigger a host of unpleasant physical and psychological symptoms that can last a few…

There’s a reason why most medications have a warning label against mixing with alcohol. In this specific instance, the danger…

How Addictive Is Cocaine? Cocaine, coke, snow, whatever you want to call it, is an addictive drug that people across…

We all wish we could know when one of our loved ones is abusing drugs so that we can act…

Fentanyl is a potent drug that is used to relieve severe pain. One example is the use of fentanyl in…

Acid, or Lysergic acid diethylamide (LSD), is a hallucinogenic drug. This means that when consumed, it causes the user to…

If you want to know how to help a meth addict, let’s start here: don’t call them a meth addict.…
Between the national opioid crisis and historically high instances of alcoholism, drug use, abuse, and addiction are common in nearly…

Over 600,000 adolescents between the ages of 12 and 17 are estimated to have had a past year illicit drug…

There are a number of different ways in which drugs can be referred to. This includes one of their street…

A woman and mother of 2 wakes up every day and begins her morning routine. She takes her women’s multivitamin…
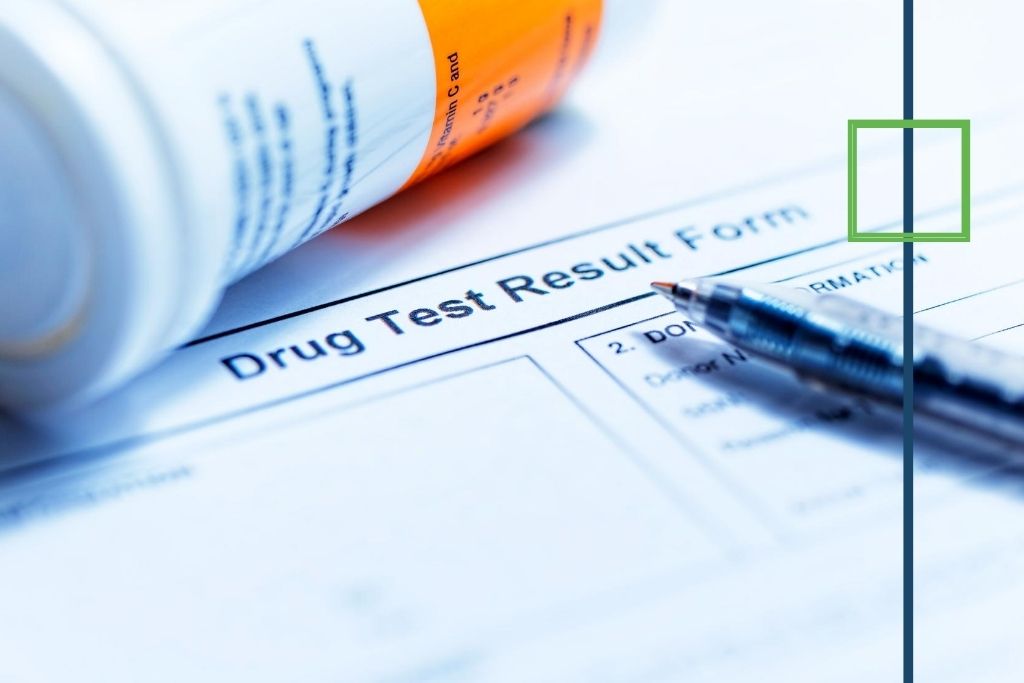
Urine drug tests are the most common method of screening for drug use. This is because urine tests are affordable,…

Whether natural or synthetic, there is an astounding array of chemical substances obtainable in the United States. While we can…
Crack cocaine, more commonly referred to by its shorthand 'crack', is a cruder form of cocaine. These illicit street drugs…

Memory loss is not just something that can occur from a major traumatic event or old age. In fact, there…
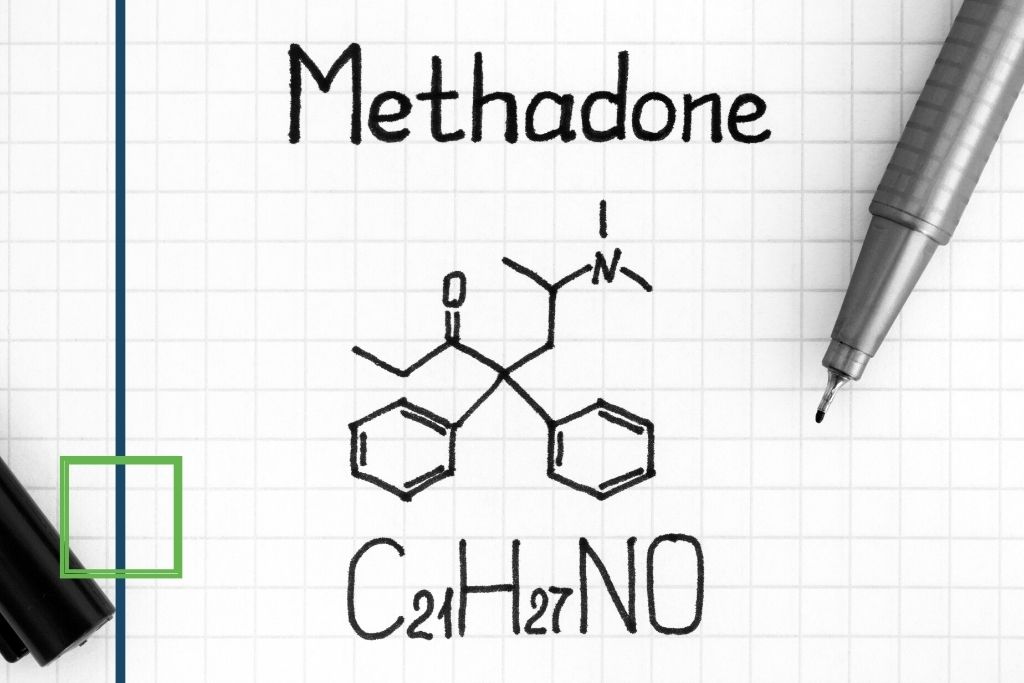
Methadone is a medication that was first synthesized in 1939. Distribution and use of the drug began within just a…